|
ACRANIA ACARDIA (TRAP
SEQUENCE) |
(Acardiac Parabolic Twin; Twin Reversed Arterial Perfusion
Sequence)
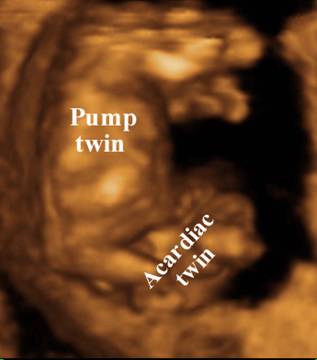
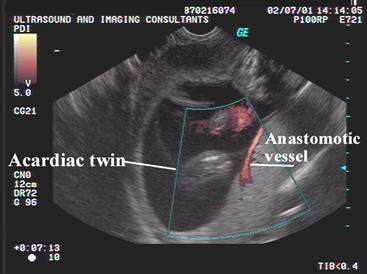
Acardiac twinning, one of the most
severe congenital malformations seen in humans, is unique to monochorionic placentation and
occurs with a reported prevalence of 1% of monozygotic twins. Its most distinctive feature, and the main focus of our
attention, is the presence of a structurally normal pump twin, which provides a
blood supply to the parasitic acardiac twin in a
retrograde, paradoxical fashion through a single superficial artery-to-artery anastomosis.
- It is thought to be an example of extreme twin-to-twin transfusion. It occurs as a sporadic event as there have been no reports of family recurrence. There are sporadic reports of chromosomal abnormalities in the acardiac and pump twin, however the surviving phenotypically normal twin usually has a normal karyotype.
- 0.3:10,000 pregnancies. 1% of monozygotic pregnancies. It has been reported in dizygotic pregnancies where the placentas are fused. May occasionally be identified in triplet and quintuplet pregnancies (1-4).
|
Normal Fetus (Pump Twin) |
|
|
|
|
|
|
Malformed Fetus
with limited Development of the Upper Body
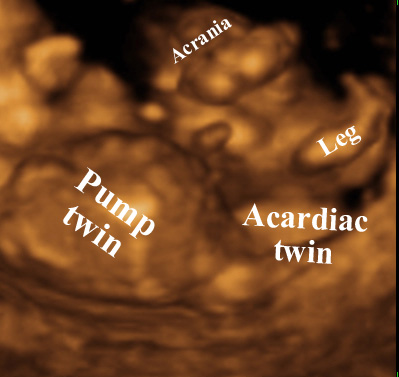
The patterns of malformations are influenced by the reversed perfusion that exists. The acardiac twin receives blood from an artery-to-artery anastomosis, and therefore receives blood that has already circulated through the pump twin and is thus poor in oxygen and nutrients. Since the richest blood arrives through the iliac arteries (via umbilical arteries), there is relative sparing of the lower extremities. Anomalies related to anoxia and poor nutrient supply increases with increased distance from the pelvis (cephalad). Blood return from the anomalous twin via it’s umbilical vein and anastomosis either with the umbilical vein of the normal twin or with venous vessels in the placenta. The original etiology suggested that reversed transfusion occurred through at least two anastomoses (artery to artery and vein to vein) may be oversimplifies and that vascular anastomoses may be more complex (6).
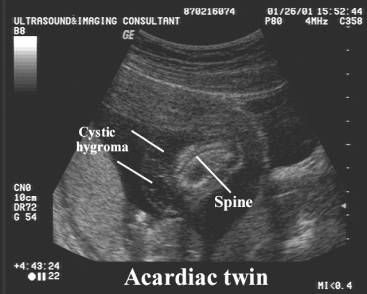
1. Usually no heart (acardia) or occasionally a micro 2 chambered heart (pseudocardia).
2. Ribs or vertebrae may be present, rudimentary, absent or dysplastic.
3. Head usually absent (occasionally a small head with holoprosencephaly, anencephaly and facial clefting)
4. Cervical spine, arms and ribs are hypoplastic or absent.
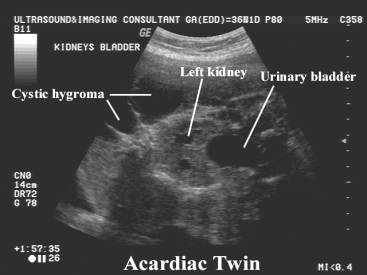
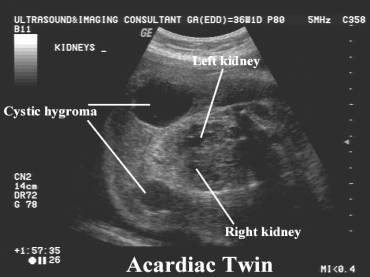
5. Pelvis and lower extremities are usually more fully formed (there may be ray deficiencies and equinovarus malformation).
6. Abdominal visceral anomalies include absence of any discernable abdominal organs; persistence of embryonic structures (urachus, aberrant vessels); absent, normal or deficient external genitalia.
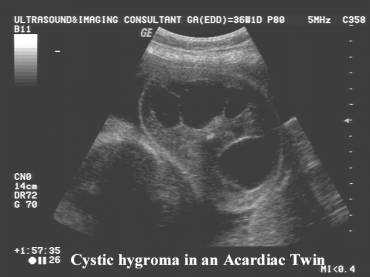
7. A large dorsal multiloculated cystic hygroma is generally present (may attain massive proportions).
8. Single umbilical artery (usually).
Classification of acardiac fetuses |
|
|
Acardius amorphous:
|
Acardius acormus:
|
|
Acardius acephalus:
|
Acardius anceps:
|
|
Case 1 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Pathological specimen of
abdominal viscera:
|
|
Case 2 |
|
|
|
|
|
|
|
|
|
|
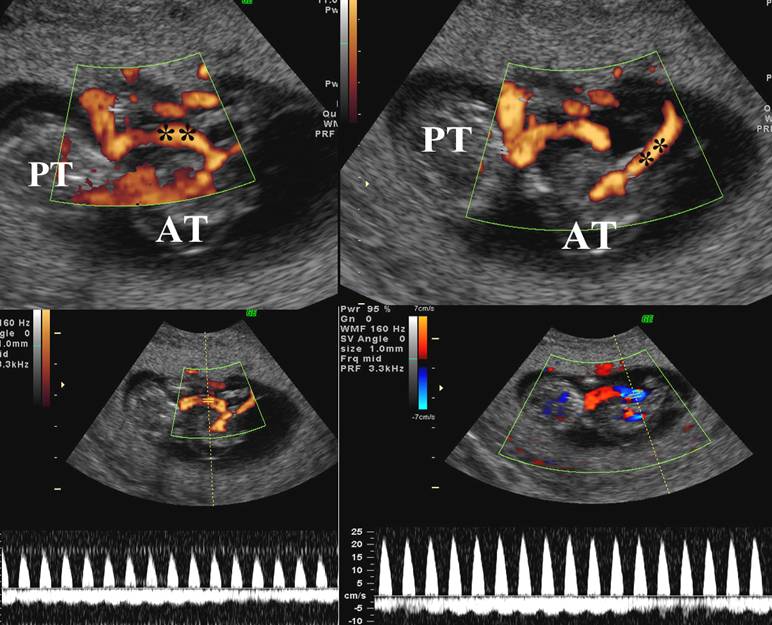
Mechanism of Development of an Acardiac Fetus
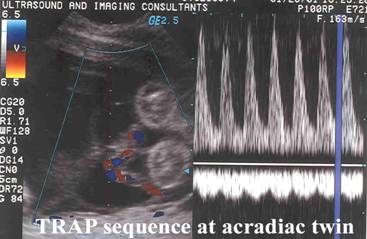
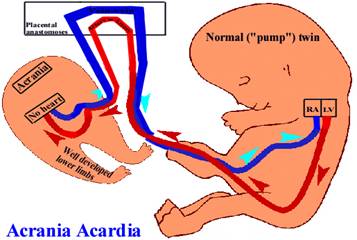
Deoxygenated blood from the pump twin travels from the heart to the placenta through the umbilical arteries. An artery-artery anastomosis in the placenta sends this poorly saturated blood in a retrograde direction through the umbilical arteries of the acardiac fetus where it enters the body through the iliac arteries. The minimal residual oxygen that is available is extracted by the tissues in the lower portion of the acardiac fetus allowing some development and growth of the lower extremities. The blood now fully desaturated flows in a retrograde direction through the upper body and head, which is poorly formed. The blood then flows back to the placenta via the umbilical vein. A vein-vein placental anastomosis completes the circulatory circuit back to the pump twin. This abnormal circulatory circuit gives rise to the alternate name to this condition: Twin reversed arterial perfusion (TRAP) sequence.
Either this vessel courses on the surface of the placenta or, occasionally, the single umbilical artery of the acardiac twin connects directly with the umbilical cord of the pump twin. The acardiac twin, therefore, lacks a functional placenta and its entire fetoplacental blood volume is confined to its own vascular tree.
|
Vascular
anastomoses in TRAP sequence – vessel on
surface of placenta |
|
|
|
|
|
|
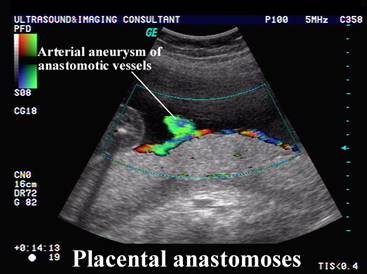
Arterial-Arterial anastomosis on the surface
of the placenta |
|
|
|
|
|
Vein-Vein anastomosis on the surface of the placenta. |
|
|
Arterial
aneurysm on surface of placenta |
|
Vascular anastomoses in TRAP sequence -
the single umbilical artery of
the acardiac twin connects directly with the
umbilical cord of the pump twin |
|
|
|
|
|
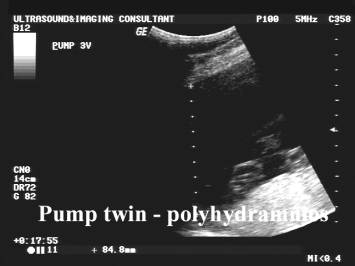
OUTCOME OF PUMP TWIN |
- Persistent state of high cardiac output, which increases renal output resulting in polyhydramnios and possible preterm labor.
- Occasionally hydrops and death (55%).
- The risk of congestive cardiac failure, polyhydramnios and preterm labor is directly related to the ratio of the weights of the pump to the acardiac twin.
- If the weight of the acardiac twin is greater than 70% than that of the pump twin:
- Preterm labor = 90%
- Polyhydramnios = 40%
- Congestive failure = 30%
- If the weight of the acardiac twin less than 70%:
- Preterm labor = 75%
- Polyhydramnios = 30%
- Congestive failure = 10%
|
REFERENCES |
- Severn CB, Holyoke EA. Human cardiac anomalies. Am J Obstet Gynecol 1973;116:358-365.
- Schinzel AAGL, Smith DW, Miller JR. Monozygotic twinning and structural defects. J Pediatr 1979;95:921-930.
- Benirschke K, Kim CK. Multiple pregnancy. N Engl J Med 1973;288:1276-1284.
- Bonilla-Musoles F, Lopez A, Pardo G et.al. Sonographische Diagnose eines Holokardius. Ultraschall Med 1987;8:185-188.
- Bonilla-Musoles F, Machado LE, Raga F, Osborne NG. Fetus acardius. J Ultrasound Med 2001;20:1117-1127.
- Shih JC, Shyu MK, Huang SF et.al. Doppler waveform analysis of the intertwin bloodflow in acardiac pregnancy: implications for pathogenesis. Ultrasound Obstet Gynecol 1999;14:375-379.
- Fouron JC, Leduc L, Grigon A et.al. Importance of Meticulous Ultrasonographic Investigation of the Acardiac Twin. J Ultrasound Med 1994, 13:1001-1004.
- Schwarzler P, Ville Y, Moscosco G et.al. Diagnosis of twin reversed arterial perfusion sequence in the first trimester by transvaginal color doppler. Ultrasound Obstet Gynecol 1999;13:143-146.