|
UTERINE SIGNS IN
ECTOPIC PREGNANCY CERVICAL ECTOPIC
PREGNANCY |
- The presence or absence of an intrauterine pregnancy must first be determined
- Discriminatory levels:
- Endovaginally a normal pregnancy should be seen when bhCG>1000 IU/L (Second International Standard).
- This level has not been fully assessed in patients with multiple gestations
- The presence of an intrauterine pregnancy virtually excludes the presence of an associated ectopic gestation, however the adnexae should always be carefully visualized. Heterotopic pregnancies in patients undergoing assisted techniques are reported as high as 1.1% (1).
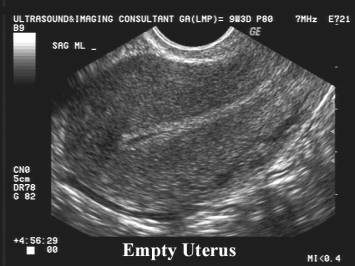
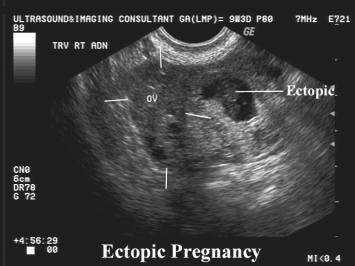
THE EMPTY UTERUS
|
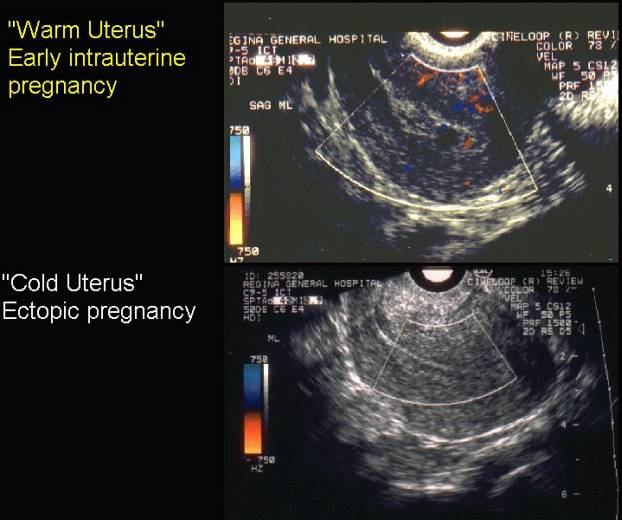
- Intrauterine pregnancy not yet visible (see discriminatory levels). "Warm uterus" - this refers to the amount of color doppler pulses at the site of trophoblastic implantation, and is found in early intrauterine pregnancies as well as in incomplete abortions i.e. signifies an intrauterine pregnancy is or was in the uterus.
|
|
- Complete abortion (sequential bhCG will demonstrate decreasing titres).
ENDOMETRIAL FINDINGS
|
- No diagnostic endometrial findings.
- Thickness of endometrium varies from thin to thick.
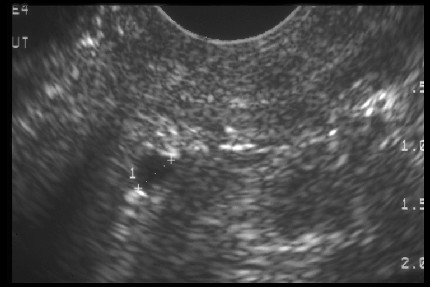
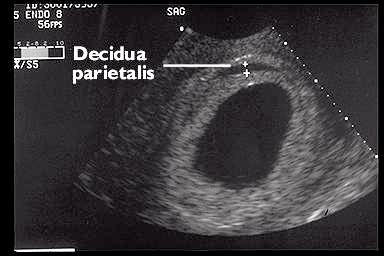
- Decidual cysts appearing at the junction of endometrium and myometrium are associated with both intrauterine and ectopic pregnancy.
|
|
Decidual cysts
appearing at the junction of endometrium and myometrium |
|
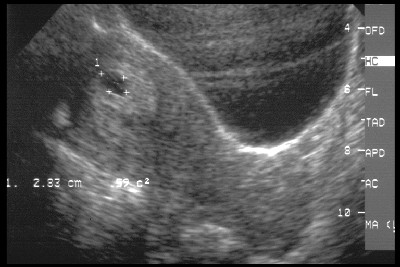
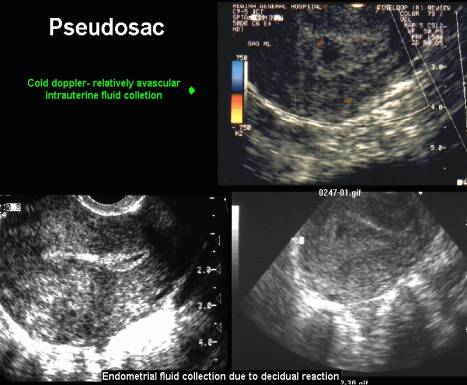
True Sac |
Pseudosac |
|
Double
decidual reaction |
Single
decidual reaction corresponding to the endometrial decidual reaction. Pseudosac
is caused by either intrauterine fluid surrounded by a thick decidual
reaction or by a detached decidual cast containing fluid centrally. |
|
|
|
|
|
|
|
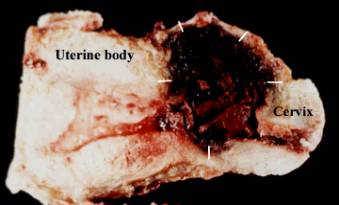
CERVICAL ECTOPIC
PREGNANCY |
ETIOLOGY
|
· Unknown
· Other factors including local cervical pathology:
o Previous dilatation and curettage (Parente et al. (2)of 31 cases of cervical pregnancy found that 25 of 31 patients had had previous curettage)
o Asherman’s Syndrome
o Previous Cesarean section
o Previous cervical or uterine surgery
o In vitro fertilization-embryo transfer (3,4).
ULTRASOUND
|
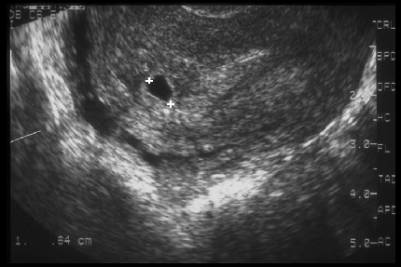
· Diagnosis of cervical pregnancy requires visualization of an intracervical ectopic gestational sac or trophoblastic mass.
· Transvaginal ultrasound improves visualization in cases of early cervical pregnancy.
· Transabdominal imaging, allows visualization of the uterus, canal and vagina in a single plane. It may be preferable in advanced cases of cervical pregnancy.
· Ushakov et al. (5) suggest that visualization of an intact part of the cervical canal between the endometrium and gestational sac reflects an intracervical placentation.

DIFFERENTIAL DIAGNOSIS
|
· Differentiation of a true cervical pregnancy from an isthmico-cervical pregnancy is important and requires demonstration of a closed internal os.
· The internal os (on a coronal view) is said to be at the level of the insertion of the uterine arteries (5).
· Thus, if the internal os cannot itself be visualized, the sac should be below the uterine artery insertion which should be identifiable.
· Cervical stage of miscarriage defined as “sliding sign” described on transvaginal scanning by Jurkovic et al. (6) which occurs when the gestational sac of an abortus slides against the endocervical canal following gentle pressure by the sonographer (this will not be seen in an implanted cervical pregnancy may also assist in the differentiation).
· Local endocervical tissue invasion by the trophoblast is also important in cervical pregnancy and it may be possible to identify the site with ultrasound. The cervical mucosa has no protection against trophoblast invasion and allows deep penetration of proliferating chorionic villi into the fibromuscular layer. The hyperechoic trophoblastic ring will be thicker in the area of invasion. It may be more difficult to visualize the remaining thinned cervical wall.
· Low resistance placental blood flow due to the trophoblastic villi, may be detected in an intracervical position confirming the site of implantation.
· Jurkovic et al. noted that a non-viable sac passing through the cervix will have no peritrophoblastic flow. However, Benson and Doubilet disputed the usefulness of color Doppler, stating the overlap of findings between miscarriage and cervical ectopic pregnancy was too great to add significant diagnostic information (7).
· Intrauterine sac with low placentation. The empty or relatively empty endometrial cavity should indicate the correct diagnosis. If a cervical mass is identified at a late stage without viable products, which with cervical pregnancy is less likely due to the favorable conditions, the margins may be irregular or ill defined due to the trophoblastic invasion. The differential diagnosis at this stage includes incomplete, missed or inevitable miscarriage, gestational trophoblastic disease, degenerative leiomyomata and cervical malignancy. The spherical shape, the empty or relatively small uterus and the closed endometrial canal and internal os will again assist in the correct diagnosis.
REFERENCES
|
- Svare J, Norup P, Grove Thomsen S et.al. Heterotopic pregnancies after in-vitro fertilization and embryo transfer: A Danish survey. Hum Reprod 1993;8:116-118.
- Parente JT, Chau Su Levy J, Legatt E. Cervical pregnancy analysis. A review and report of five cases. Obstet Gynecol 1983; 62: 79
- Shinagawa S, Nugayama M. Cervical pregnancy as a possible sequela of induced abortion. Am J Obstet Gynecol 1969; 105: 282-4
- Eblen AC, Pridham DD, Tatum CM Jr. Conservative management of an 11 week cervical pregnancy a case report. J Reprod Med 1999; 44: 61-4
- Ushakov FB, Elchalal V, Aceman PJ, Schenker JK. Cervical pregnancy. past and future. Obstet Gynecol Sur 1996; 52: 45-59
- Jurkovic D, Hacket E, Campbell S. Diagnosis and treatment of early cervical pregnancy: a review and a report of two cases treated conservatively. Ultrasound Obstet Gynecol 1996; 8: 373-80
- Benson CB, Doubilet PM. Strategies for conservative treatment of cervical ectopic pregnancy. Ultrasound Obstet Gynecol 1996; 8: 371-2