|
AMNIOTIC BAND SYNDROME (ABS) |
The
amniotic band syndrome is a group of sporadic congenital anomalies
characterized by amputations, constriction bands, pseudosyndactylism and
multiple craniofacial, visceral and body wall defects. It occurs in 1 in 1200
to 1 in 15 000 live births (1). Although the exact cause of the syndrome
is not known, early rupture of the amniotic membrane resulting in bands that
insert on the body of the fetus is the most accepted view (1).
|
Sonographic appearance of membrane |
Relationship to Fetus
|
|
|
* Thin aberrant bands of tissue attached to the fetus. * Fetal deformities. but
characteristic fetal deformities in a
non-embryonic distribution is highly suggestive. |
*
Commonly
associated with fetal deformities. |
|
|
Relationship to Placenta |
Timing
|
Pathology/Etiology
|
|
* Usually none. |
* Early amnion rupture is thought to result in ABS due to the adhesive
nature of the external amnion and chorion. |
* Entrapment of fetal parts is the result of rupture
of the amnion and development of fibrous mesodermal bands on the chorionic
side of the amnion. |
|
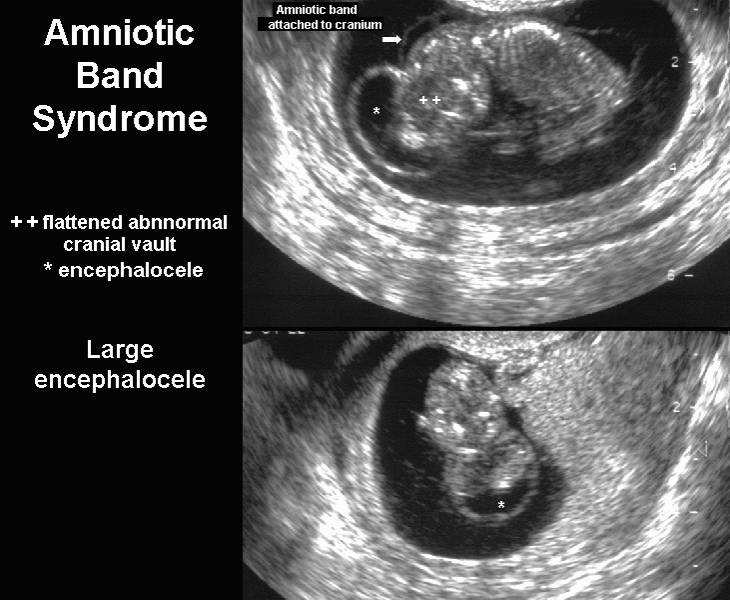
Central
nervous system – large encephalocele |
|
|
|
|
|
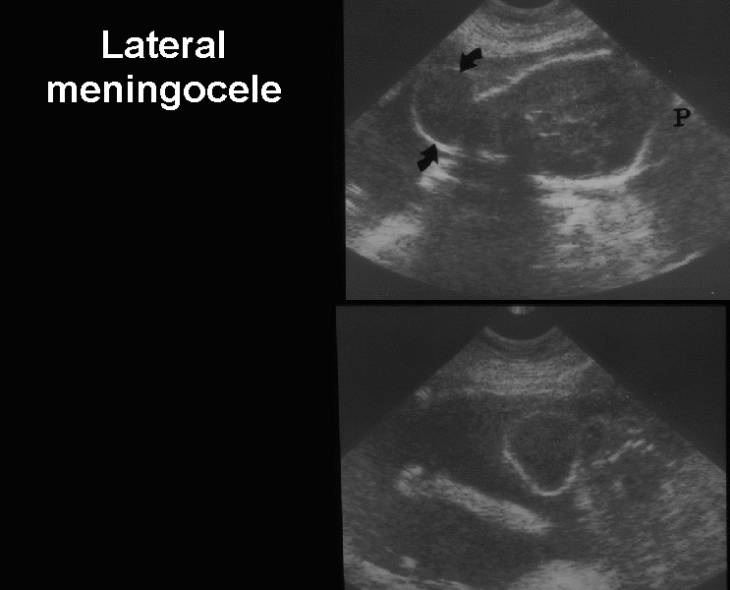
Central
nervous system – lateral meningocele |
|
|
|
|
|
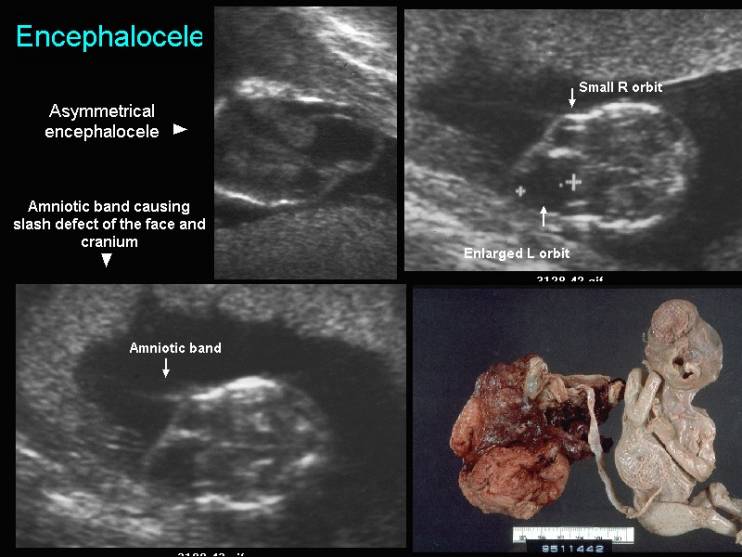
Central
nervous system and face – enecephalocele, large orbit, abnormal mouth
and nose due to slash defects. |
|
|
|
|
|
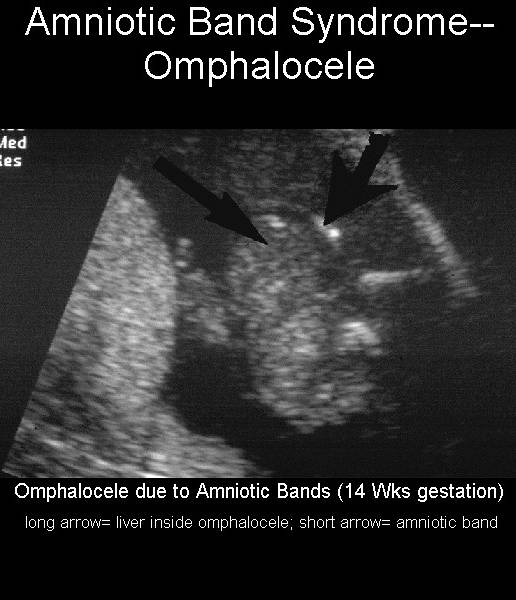
Abdomen
– Omphalocele (long arrow delineated the omphalocele; short arrow
represents the covering membrane). the fetus also had anencephaly. |
|
|
|
|
|
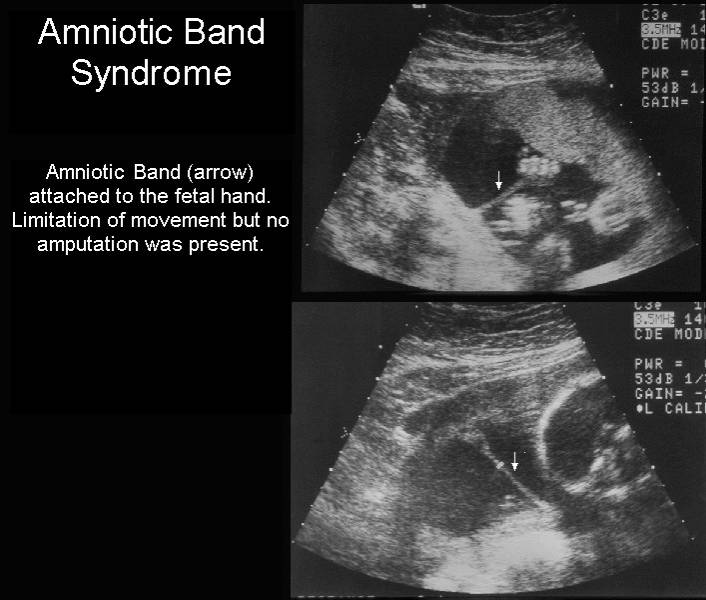
Limbs –
band attached to the hand. No defect seen |
|
|
|
|
|
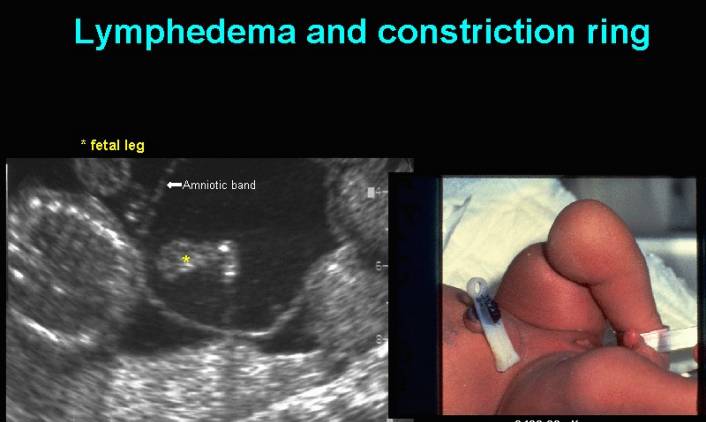
Limbs –
constriction defect involving the thigh |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Video of Amniotic Band Syndrome
|
|
|
|
|
|
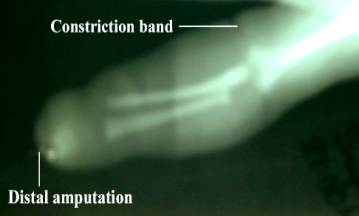
The most accepted theory to explain the pathogenesis of the amniotic band syndrome was presented by Torpin (1). According to his theory, the primary event is a rupture of the amniotic membrane and its detachment from the chorion with amniotic fluid leaking through the tear. As a result, the fetus can move digits or limbs through this tear and exit the amniotic cavity (partially or completely). The outer surface of the amnion, and to a lesser degree the naked chorion, produce mesodermic fibrous strings which may entangle and entrap different fetal organs, leading to constriction and amputation anomalies. These deductions agree with the increased frequency of constriction bands located more distally on the digits, hands and feet, as well as with the varying severity of constrictions, ranging from slight grooves in the skin to actual amputation of the digit or limb (2). However, this theory does not explain the association of amniotic bands with damage to internal organs and other severe anomalies. Bronshtein and Zimmer (3) challenged the concept that amniotic bands amputate fetal organs. Over the period of a decade, they observed many cases of finger and limb amputations without ever visualizing attachment of amnion at the exact site of amputation. They also wondered why amputations always seem to occur transversely and discussed the possibility of a primary teratogenic insult.
REFERENCES |
1. Torpin R. Amniochorionic mesoblastic fibrous strings and amniotic bands: associated constricting fetal malformations or fetal death. Am J Obstet Gynecol 1965; 91: 65–75
2. Browne D. The pathology of congenital ring constrictions. Arch Dis Child 1957; 32: 517–9.
3. Bronshtein M, Zimmer EZ. Do amniotic bands amputate fetal organs? Ultrasound Obstet Gynecol 1997; 10: 309–11