|
FETAL GALLBLADDER
(1,2) |
The gallbladder, one of the organs among the extrahepatic biliary duct system, arises from the hepatic diverticulum in the fourth week of gestation, the cystic duct and gallbladder primordium being visible as a bud from the side of the diverticulum (1).
At the beginning of the fifth week, the extrahepatic duct system, the gallbladder, cystic duct, hepatic ducts, common bile duct and pancreatic duct are demarcated. During this stage, the future duct system becomes a solid cord of cells.
Re-establishment of the lumina of the ducts begins in the sixth week with the common duct, and progresses slowly in a distal direction.
The lumina extends into the cystic duct by the seventh week, but the gallbladder remains solid until the 12th week (2).
Bile is formed by the fetal hepatic cells during the 12th week of gestation, and enters the duodenum via the bile duct after the 13th week of gestation (1).
- Pear shaped (tear drop), ovoid, round or disc shaped.
- Anechoic/hypoechoic.
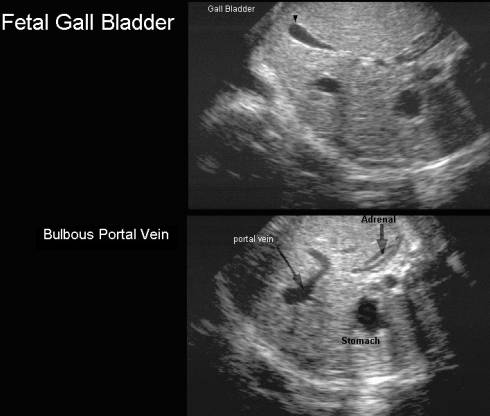
- Between left and right lobes of the liver on transverse scans.
- Parallel and to the right of the portal sinus.
- At a 30-45 degree angle to the umbilical vein.
- Can occasionally be septated or bilobed.
|
|
|
Normal gallbladder length (Table) –
Chan et.al.
1995
Normal gallbladder transverse diameter
(Graph) – Chan et.al. 1995
Gallbladder length – Chan et.al. 1995
Gallbladder transverse diameter –
Chan et.al.
1995
· Growth of the fetal gallbladder has been reported between 15 weeks gestational age and term (4,6). Hata et al., (4)and Chan et al (6), determined that the fetal gallbladder size increased linearly until 30 weeks of gestation, and became constant. Goldstein et al (3) described a linear growth function between fetal gallbladder size and gestational age was observed throughout pregnancy
·
Physiological periodic
emptying is believed to occur.
o In adults, gallbladder contraction is usually regulated by cholecystokinin, a polypeptide hormone that is secreted by duodenal mucosa cells after local stimulation by peroral meals.
o Although pure glucose is also capable of inducing gallbladder contractions (albeit to a lesser degree), little is known about the function of cholecystokinin or effect of glucose on fetal gallbladder contractility in humans.
o The fetal gastric and duodenal mucosa is capable of producing many important enzymes at the end of pregnancy, and therefore cholecystokinin production in fetal duodenal cells may also be possible (7).
o In the guinea pig model, cholinergic and cholecystokinin receptors were present and functional on gallbladder smooth muscle before birth (8).
o It was also demonstrated that the size of fetal gallbladder remained constant for 3 h after maternal test meals (5). A later report (3) confirmed that fetal gallbladder dimensions remained relatively constant for 3 h periods of evaluation, although the gestational age varied.
o
In a study by Tanaka et.al.
(9) the daily change in fetal gallbladder
volume showed a typical sinusoidal pattern, and the cycle of
gallbladder volume change was constant during pregnancy. The
contractility rate increased curvilinearly with
advancing gestation. This finding may suggest a reason for the
decrease in association between fetal gallbladder volume and
functional capacity with advancing gestational age. Moreover, the
phase difference of each fetal gallbladder contractility cycle was
specific to each fetus, and unaffected by
maternal feeding.
o Pathological
gallbladder dilatation therefore should not be diagnosed on the
basis of a single observation of a prominently distended fetal
gallbladder.
Contractility of the fetal gallbladder monitored by ultrasonography during pregnancy has been reported (3,5), and the changes in fetal gallbladder size were not significant during the observation period.
However, the duration of observations reported in both studies was rather short (only 3 h), and both studies ignored the phase difference of each fetal gallbladder contractility cycle.
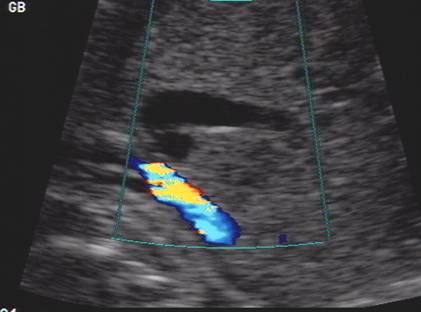
- Differentiate from the umbilical vein which is:
- Tubular.
- Inserts centrally into the fetal abdominal wall.
- Pulsed doppler demonstrates flow within the vein.
- May be confused with a bulbous portal vein (normal variant).
|
|
- Normal variants.
|
Phrygian cap –(folding of the fundus of the gallbladder |
|
|
|
|
|
Megacholecystis
– large gallbladder (28 wks GA) |
|
|
|
|
|
Megacholecystis
– postnatal ultrasound on Day 14 |
|
|
|
|
- Always seen by week 15 GA.
REFERENCES |
1.
2. Gray,
S.W. and Skandalakis, J.E. (1972) Embryology for Surgeons. W.B.Saunders,
3. Goldstein I, Tamir A, Weisman A et.al. Growth of the fetal gallbladder in normal pregnancies. Ultrasound Obstet Gynecol 1994;4:289.
4. Chan
L, Rao BK, Jiang Y et.al. Fetal gallbladder growth and development during
gestation. J Ultrasound Med 1995;14:421-425.
5. Jouppila
P, Heikkinen J, Kirkinen P.
Contractility of maternal and fetal gallbladder: An ultrasonic study. J Clin Ultrasound 1985;13:461.
6. Hata,
K., Aoki, S., Hata, T. et al. (1987) Ultrasonographic
identification of the human fetal gallbladder in utero. Gynecol. Obstet. Invest., 23, 79–83
7. Kimura,
R. and Warshaw, J. (1981) Intrauterine
development of gastrointestinal tract function. In Lebenthal,
E. (ed.), Textbook of Gastroenterology
and Nutrition in Infancy. Raven Press,
8. Denehy, C.M. and Ryan, J.R. (1986) Development
of gallbladder contractility in the guinea pig. Pediatr. Res., 20,
214–217
9. Tanaka
Y, Senoh D, Hata T. Is
there a human fetal gallbladder contractility during
pregnancy. Human Reprod 2000;15:1400-1402.