|
TWIN-TWIN TRANSFUSION
SYNDROME (TTTS) |
Definition,
General Comments and Vascular Anastomoses
ULTRASOUND IN THE FIRST TRIMESTER |
TTTS is a slowly progressive disease. Initial presentation as early as 13 weeks' gestation has been reported, but it usually occurs in the second trimester. Routine obstetric ultrasonography will usually allow for the visualization of TTTS at 17 to 26 weeks.
Diagnostic criteria include;
- Monochorionic gestation .
- Nuchal translucency measurement >3 mm at 10-14 weeks' gestation (with normal chromosomes).
- Poor crown-rump length growth in one fetus.
- Membrane folding at 10-13 weeks' gestation .



ULTRASOUND IN THE SECOND AND THIRD TRIMESTERS |
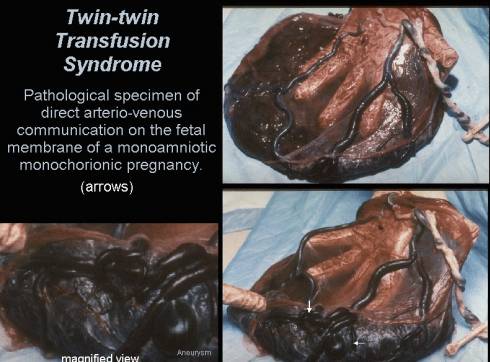
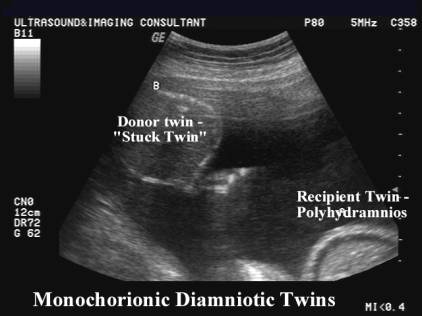
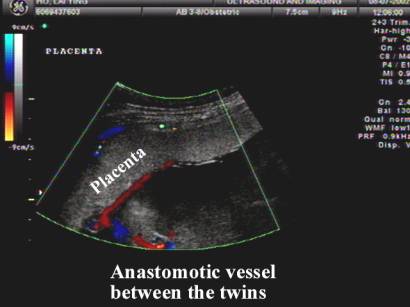
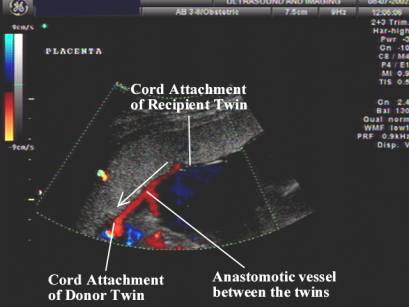
Abnormal vascular connections and the resultant disparate sharing of blood flow occur in monochorionic twins. The twin-twin transfusion syndrome results from arterio-venous connections (one of the many vascular anastomoses) that occur in monochorionic placentas and may lead to a physically "stuck" twin. The vast majority of monochorionic placentas have vascular anastomoses, however only 15-30% actually result in the twin-twin transfusion syndrome.
- Monochorionic twins.
- Fetuses have the same sex (9,10).
- Biometric disparities on a first or second trimester scan.
- Different fetal sac sizes.
- Different quantity of
amniotic fluid surrounding each fetus (One sac with oligohydramnios, deepest vertical pocket 2.0 cm
One sac with polyhydramnios, deepest vertical pocket 8.0 cm). - Identification of placental confluence (9). Discordant echogenicity of the donor and recipient placental areas has been reported (7).
- Persistent Urinary Bladder Findings
- Small or no bladder visualized in twin with oligohydramnios.
- Large bladder visualized in twin with polyhydramnios.
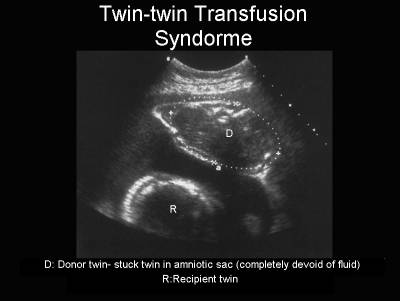
- Appearance of a stuck twin
- Hydrops fetalis (presence of one or more of the following in either twin): skin edema (5-mm thickness), pericardial effusion, pleural effusion, ascites.
- Membrane folding at 14-17 weeks' gestation
- Inter-twin hemoglobin difference of 5 g/dl or more (9).
- Inter-twin birth weight difference of greater than 15-20% (5).
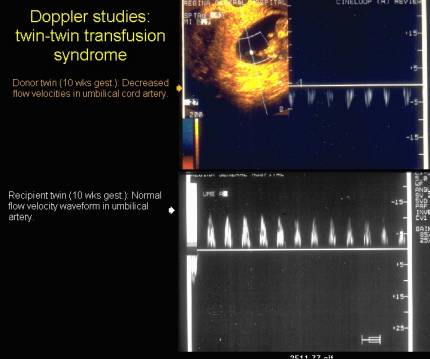
- Different size umbilical cords. Doppler velocimetry of the umbilical artery with an inter-twin difference in S/D ratio of greater than 0.4 (9).
- Artery-to-vein shunt involving the fetal surface placental vessels.
|
|
- Fetal hydrops or cardiac failure may be present.
- Increased nuchal translucency
- Most workers seem to agree that the above diagnostic criteria may be present, but the diagnosis should be restricted to monochorionic twins with gross discordance of amniotic fluid volume in the second or early third trimester (7).
Donor Twin |
Recipient Twin |
||||||||||||||||||
|
Single placenta Thin membrane Same sex fetuses Discordant growth |
|||||||||||||||||||
|
Oligohydramnios (60%) |
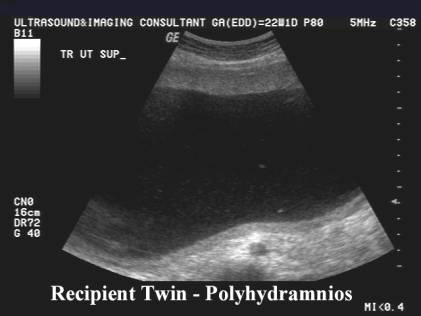
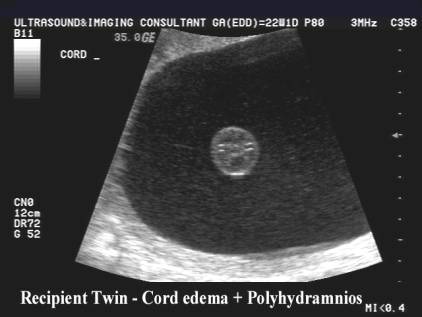
Polyhydramnios - moderate to severe |
||||||||||||||||||
|
|
|
||||||||||||||||||
|
Small / empty bladder |
Large bladder |
||||||||||||||||||
|
"Stuck twin" - pinned to the side
|
Cardiomegaly due to increased
perfusion and volume overload |
||||||||||||||||||
|
No free movement in the
gestational sac due to the oligohydramnios |
Moves freely in the hydramniotic
gestational sac |
||||||||||||||||||
|
Amnion may not be seen as it
lies in contact with the fetal body parts and can't be distinguished as a
membrane separating twins. |
|
||||||||||||||||||
|
Anemia and hypovolemia |
Polycythemia and plethora |
||||||||||||||||||
|
Morphologically normal |
Fetal papyraceus |
||||||||||||||||||
|
|
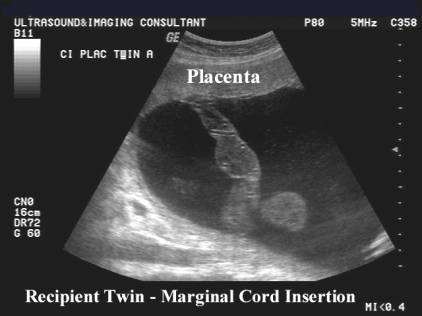
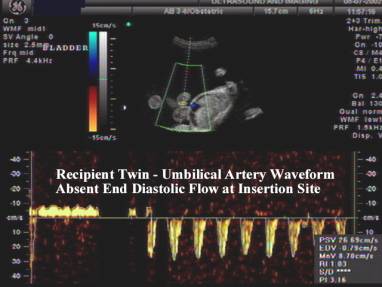
Velamentous cord insertion
(64%) |
||||||||||||||||||
|
|
|
||||||||||||||||||
|
|
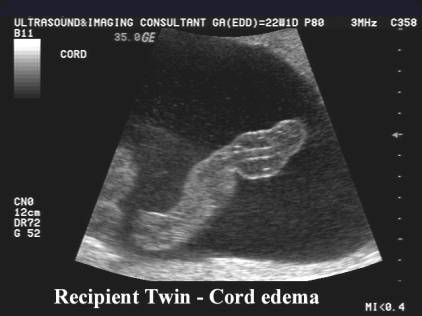
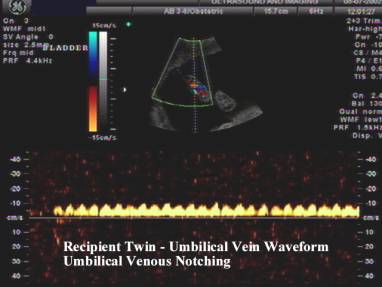
Cord Edema |
||||||||||||||||||
|
|
|
||||||||||||||||||
|
Fetal hydrops rare |
Fetal hydrops in 10-25% |
||||||||||||||||||
|
|
|
||||||||||||||||||
Vascular Anastomoses in the Placenta
|
|||||||||||||||||||
|
|
|
||||||||||||||||||
|
|
|
||||||||||||||||||
|
“Coccoon sign” – this is
thought to be a variant of the classic stuck twin, characterized by a donor
fetus with severe oligohydramnios being enveloped by intact, collapsed
dividing membranes, yet located away from the periphery of the intrauterine
cavity. The fetus is anchored to the periphery by a tether of folded
membranes, similar to a cocoon (14). |
|
||||||||||||||||||
|
|||||||||||||||||||
STAGING OF TTTS BASED ON TREATMENT (8) |
TTTS has been defined as a deep vertical pocket in the recipient twin of >8 cm and in the donor twin <2 cm.
Stage 1 – donor bladder visible
Stage 2 – donor bladder not visible (normal dopplers: UA, UV, Ductus venosus).
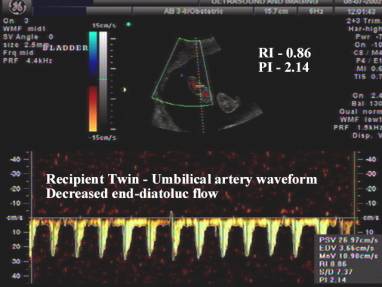
Stage 3 – critically abnormal dopplers (absent or reversed diastolic flow in the UA, UV or intrahepativ vein pulsations, reversal of a wave of ductus venosus).
Stage 4 - hydrops
Stage 5 - demise
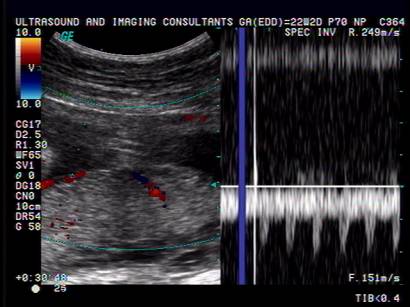
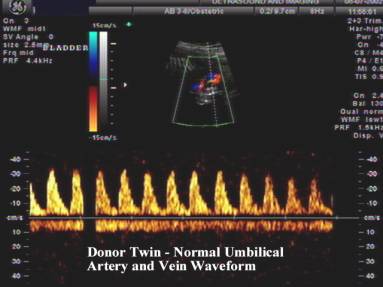
DOPPLER STUDIES |
Doppler investigations of the arterial vessels and ductus venosus, IVC and right hepatic vein, tricuspid and mitral ventricular inflow performed on the venous side revealed decreased blood flow velocities.
Mean values of atrioventricular flow velocities showed a significant
decrease in the donor group (1).
|
Donor Twin |
Recipient Twin |
|
|
|
DIFFERENTIAL DIAGNOSIS |
IUGR of one twin. To distinguish this from the twin-twin transfusion syndrome
the recipient twin does not usually have polyhydramnios or congestive cardiac
failure. IUGR may occur in dichorionic pregnancies whereas the twin-twin
transfusion syndrome only occurs in monochorionic pregnancies.
OUTCOME |
Perinatal mortality of 71% (when diagnosed prior to 26 weeks).
REFERENCES |
- Sharma S, Gray S, Guzman ER et.al. Detection of twin-twin transfusion syndrome by first trimester ultrasonography. J Ultrasound Med 1995;14:635-637.
- Fox H. Pathology of the placenta. Philadelphia: W B Saunders 1978:73-94.
- Brown DL, Benson CB, Driscoll SG et.al. Twin-twin transfusion syndrome: sonographic findings. Radiology 1989;170:61-63.
- Chescheir NC, Seeds JW. Polyhydramnios and oligohydramnios in twin gestations. Obstet Gynecol 1988;7:882-884.
- Whittman BK, Baldwin VJ, Nichol B. Antenatal diagnosis of twin transfusion syndrome by ultrasound. Obstet Gynecol 1981;58:123-127.
- Hecher K, Ville R, Snijders R, Nicolaides K. Doppler studies of the fetal circulation in twin-twin transfusion syndrome. Ultrasound Obstet Gynecol 1995;5:318-324.
- Frisch L, Arava J, David H
et.al. Severe twin-to-twin transfusion syndrome: a new sonographic feature
of the placenta. Ultrasound Obstet Gynecol 1997;10:145-146.
- Quintero RA, Bornick PW, Morales WJ et.al. Stage-based treatment of twin-twin transfusion syndrome: preliminary study. 10th World Congress of Ultrasound in Obstetrics and Gynecology 2000; Zagreb, Croatia.
- Blickstein I. The twin-twin transfusion syndrome. Obstet Gynecol 1990;76:714-722.
- Brennan JN, Diwan RW, Rosen V et.al. Feto-fetal transfusion syndrome: prenatal ultrasonographic diagnosis. Radiology 1982;143:535-536.
- Bajoria R, Wigglesworth J, Fisk NM. Angioarchitecture of monochorionic placentas in relation to the twin-twin transfusion syndrome. Am J Obstet Gynecol. 1995;172:856-863.
- Machin G, Still K, Lalani T. Correlations of placental vascular and clinical outcomes in 69 monochorionic twin pregnancies. Am J Med Genet. 1996;61:229-236.
- Bajoria R. Abundant vascular anastomoses in monoamniotic versus diamniotic monochorionic placentas. Am J Obstet Gynecol. 1998;179:788-793.
- Quintero RA, Chmait RH. The cocoon sign: a potential sonographic pitfall in the diagnosis of twin-twin transfusion syndrome. Ultrasound Obstet Gynecol 2004;23:38-41.