|
THE ABNORMAL
THYMUS |
The thymus gland develops from the ventral portion of the third branchial pouch as tubular primordiums that elongate caudally and fuse at the midline, losing their connection with the pharynx and leaving the definitive thymus in the mediastinum.
The thymus is the first developing lymphoid organ. Normal peripheral lymph
nodes depend on seeding by small lymphocytes from the thymus. The thymus
reaches its greatest size at puberty, after which time it undergoes slow
involution and both cortical and T lymphocytes are reduced in peripheral blood.
ANOMALIES OF THE THYMUS |
- Cervical thymic cysts may form from persistent remnants of the tubular upper end of the primitive organ. This is an extremely rare clinical condition.
- Undescended thymus can be bilateral, but it is more commonly unilateral on the left side. Undescended thymus usually is diagnosed in childhood.
- Accessory thymus body along the line of embryonic descent is common but not clinically significant (may be found in 25% of the population).
- Thymic agenesis is an autosomal recessive disease often associated with agenesis of the parathyroid glands (DiGeorge syndrome), which leads to early death from infections or cardiac defects. Thymus and parathyroid transplant are the only possible treatment.
- Link to thymic aplasia and 22q11.2 microdeletion (congenital heart disease) The thymus may be used as a sonographic marker to identify a group with CHD in whom targeted examination of del.22q11.2 is indicated.
- In thymic aplasia the thymus is small. Usually, reticular cells and large lymphocytes are present without the small lymphocyte and Hassall bodies. Thymus and fetal liver implants to reconstitute T- and B-cell function has met with some success.
- Thymic hyperplasia: Hyperplasia is an increase in the volume of the thymus gland by formation of new cellular elements in a normal microscopic arrangement. Two morphological types exist—true hyperplasia and lymphofollicular hyperplasia. True hyperplasia is characterized by an increase in both size and weight of the thymus. Thymic hyperplasia is a very rare pathology that presents clinically or radiologically as mediastinal mass.
Three clinicopathological subtypes are identified as follows:
1. Massive thymic hyperplasia
o This is a rare pathological finding with only a few well-documented cases. Enlargement of the thymus, however, is common in infancy.
o The cause is unknown; it may be due to thymic hyperfunction or dysfunction related to the endocrine activity of the gland.
o Patients usually present with symptoms of irritation of the mediastinal structures; symptoms may range from none to respiratory distress.
2. Thymic rebound in childhood and adolescence
o This is described in a number of conditions, such as recovery from severe thermal burns, cardiac surgery, tuberculosis, following treatment for different malignancies, and after discontinuation of oral steroids.
o The functionally active thymus in childhood and adolescence may be susceptible to the fluctuation in corticosteroids levels, which is thought to be a causative factor in thymic hyperplasia (reversal of elevated endogenous corticosteroids in severe burns, withdrawal of exogenous corticosteroids in malignancy treatment).
o Patient age ranges from 2-12 years. All reported cases were detected on routine chest x-ray with no other clinical or laboratory positive finding.
o After malignancy, thymic hyperplasia could be confused radiologically with recurrence or metastasis.
3. Others:
Thymic hyperplasia has been reported in association
with sarcoidosis and endocrine abnormalities (thyrotoxicosis, hypothyroidism,
|
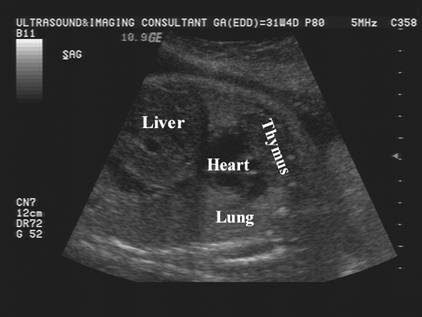
Thymic
hyperplasia (unknown etiology). Resolved postnatally. |
|
|
|
|
|
|
|
|
|
|
REFERENCES |
1. Weller GL Jr: Development of the thyroid, parathyroid, and thymus gland in man. Contrib Embryol 1933; 141: 93-139.
2. Al-Shihabi BM, Jackson JM: Cervical thymic cyst. J Laryngol Otol 1982; 96(2): 181-189
3. Kacker A, April M, Markentel CB, Breuer F: Ectopic thymus
presenting as a solid submandibular neck mass in an
infant: case report and review of literature. Int J Pediatr Otorhinolaryngol 1999;
49(3): 241-245
4. Levine
GD, Rosai J: Thymic
hyperplasia and neoplasia: a review of current
concepts. Hum Pathol 1978; 9(5): 495-515