|
TETRALOGY OF FALLOT |
Tetralogy of Fallot has four major components:
· Pulmonary valve stenosis
·
valvular in 25% of the cases,
·
infundibular in 25%, A fibromuscular or fibrous
hypertrophy of the infundibular region can be seen in the infundibular
stenosis.
·
both valvular and infundibular in 50% of the
cases.
· highly variable, from mild stenosis to cases in which pulmonary valve atresia is present. These cases are called “pseudotruncus”, since they functionally behave as a common truncus
·
The pulmonary stenosis may be progressive
and can progress all the way to pulmonary valve atresia at birth.
· High interventricular septal defect
·
perimembranous and usually wide
· Aortic root overriding the ventricular septal defect
·
Concentric hypertrophy or the right ventricle.
TYPES OF TETRALOGY |
Four types of Fallot have been described depending on
the severity or extent of the anatomical defects.
- The
“extreme” Fallot or “pseudotruncus”:
·
pulmonary
stenosis is so severe that the pulmonary artery is almost atresic or absent.
- The
“classic” Fallot:
·
pulmonary
stenosis and overriding of the aorta above the ventricular septal defect can be
seen.
- The
“pink” Fallot:
·
a small
defect is present.
·
mild
pulmonic stenosis and a discrete overriding of the aorta over the
interventricular septal defect.
- The
“pentalogy” of Fallot:
·
an interauricular septal defect is seen in
addition to the four typical components.
PREVALENCE |
·
Tetralogy of Fallot represents 15% of all the
congenital heart disease.
·
In a recent study by Boudjemline et al., in a
series of 337 cases of conotruncal heart disease:
1. tetralogy of Fallot - 56% of these cases
2. vascular
malposition 16%
3. coarctation
with or without interruption of the aortic arch 14%
4. truncus
arteriosus 9%
5. agenesis
of the pulmonary valves 5%
·
Sex ratio:
Slight predominance of males over females.
ETIOLOGY |
Several genes, separately or in combination, could contribute to these defects. The 22q11 deletion has been associated with congenital conotruncal heart defects, as well an intrafamilial variability of cardiac involvement. There is a reported case of monozygotic twins, both with tetralogy of Fallot, in whom prenatal diagnosis found 22q11 micro deletion.
Alcohol, anti-convulsivants, thalidomide and maternal
hyperphenylalaninemia and phenylketonuria have been described as teratogens to
tetralogy of Fallot
PATHOGENESIS |
- Tetralogy of Fallot is due to an abnormal embryological development of the heart in which an unequal conotruncal division results in a small pulmonary artery and a great aortic artery.
- The
incomplete embryologic rotational process of the conotruncal septum
explains the lack of alignment of this septum with the interventricular
septum in tetralogy of Fallot. The incomplete rotational process of the
aortic artery explains its dextroposition, its overriding location above
the interventricular septum and its relationship with the right ventricle.
- The
normal rotational process of the conotruncal septum does not take place
the way it should, and a lesser than 180-degree rotary motion is
responsible for the dextroposition of the aortic artery.
- The
pulmonary artery remains in an anterior position in relation to the aorta
(this differentiates tetralogy of Fallot from complete transposition of
the great vessels, where the position of the pulmonary and aortic arteries
is inverted).
- Under
normal circumstances one septum is continuous with the other. The abnormal
alignment process produces a defect of tissue between the septa, causing
the interventricular communication.
- Pulmonary
infundibular stenosis is at least partly due to anterior deviation of the
infundibular septum, which in itself narrows the subpulmonary outflow
tract. This furthers the malalignment of the septa.
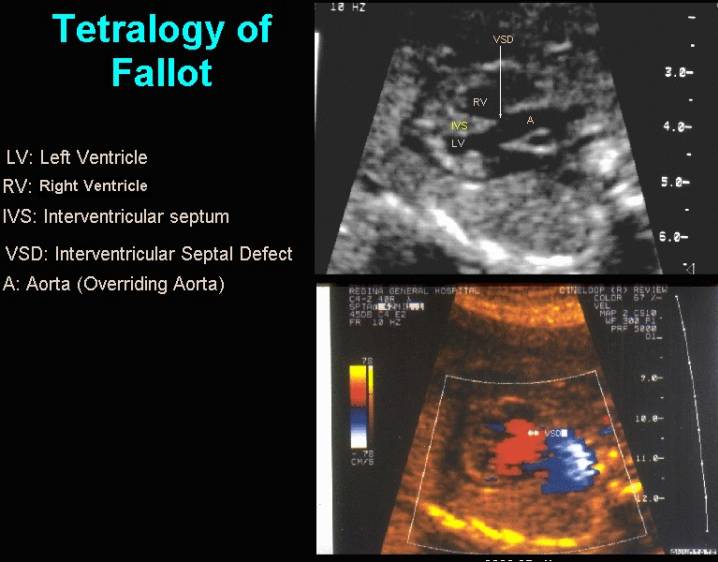
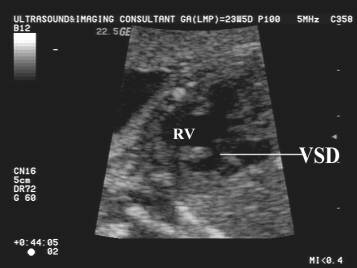
ULTRASOUND |
- The four-chamber view may look normal if the interventricular defect and overriding aorta is not seen.
- Dilated aorta overriding the interventricular septum (1,2). Beware of a common artifact that resembles overriding aorta (3).
- Aortic root dilatation, not seen in all cases, has been considered a marker of tetralogy offallot, but a normal size does not exclude the diagnosis.
- Perimembranous VSD.
- Mildly stenotic RV outflow tract.
- No RV hypertrophy in the mid second trimester (develops after birth).
- Inverse relationship between the size of the ascending aorta and pulmonary artery (often a marked disproportion).
- A large aortic root is an important diagnostic clue (4).
- Color
Doppler may demonstrate:
- Reverse
flow in the ductus arteriosus to the main pulmonary artery
(ductal-dependent circulation, which denotes poor prognosis).
- In
pulmonary stenosis and atresia, the stenotic jet, even small, is
identified by demonstration of high velocities and turbulence in the main
pulmonary artery.
- The
overriding of the aorta with blood entering from both ventricles into the
aorta is visible as a “Y” shaped image in color Doppler
during the systolic phase.
- Pulmonary
artery stenosis is not always present at initial ultrasound examination,
but this finding can develop or worsen during in-utero life.
- Main
pulmonary artery size, main pulmonary artery/aortic diameter ratio and
pattern of pulmonary artery growth may be predictive of the severity of
postnatal pulmonary outflow obstruction. Pulmonary artery atresia and
progressive pulmonary artery stenosis can develop in utero in some
fetuses with tetralogy of Fallot.
- Doppler
studies demonstrate increased peak velocities in the pulmonary artery,
due to the RV outflow tract obstruction (stenosis).
- Doppler
studies may demonstrate no flow in the pulmonary artery if complete
atresia is present.
- During the prenatal period, the concentric hypertrophy of the right ventricle is not seen.
- Cardiac failure is never seen in fetal life unless there is an absent pulmonary valve present (massive regurgitation to the RV and RA).
|
Case 1 |
|
|
|
|
|
Case 2 |
|
|
|
|
|
|
|
- Hydrops
fetalis and polyhydramnios can occasionally be seen, especially in severe
cases with absent pulmonary valve (which occurs in 3-6% of patients with
tetralogy of Fallot) and pulmonary artery aneurysm, in which the
mediastinal structures can be compressed.
The aneurysm may be seen as a cystic, pulsatile dilatation, without
definite valve echoes.
DIFFERENTIAL DIAGNOSIS |
- VSD. In cases of minor forms of right outflow tract obstruction and overriding aorta, differentiation may be difficult.
- Truncus arteriosus. In those cases in which the pulmonary artery is not imaged, differentiation between pulmonary atresia with VSD and truncus may be extremely difficult.
- Pseudo-overriding of the aorta
- Double outlet right ventricle.
ASSOCIATIONS |
- Bicuspid aortic valve (40%).
- Left pulmonary artery stenosis (40%).
- Absent pulmonary valve (2%).
- Right-sided aortic arch (35%).
- Left superior vena cava.
- Absent ductus arteriosus (15%).
- ASD (25%)
- Absent pulmonary valve with pulmonary aneurysm
- Tracheo-esophageal fistula.
- Down syndrome.
- Forked ribs, scoliosis.
- Coronary artery anomalies in 10% (single right coronary artery or left anterior descending coronary artery arises from right coronary artery).
- CHARGE association.
- Other reported anomalies
include Prune Belly syndrome and
DiGeorge sequence.
- Abnormal karyotype in 8%
of all cases
- Azancot et al. in a recent study of 44 cases of non-isolated tetralogy of Fallot, found genetic anomalies in 18 of the fetuses (10 trisomies, including five trisomies 21 and 5 structural abnormalities including 2 micro-deletions 22q11 and 1 deletion of chromosome 8p23.1 and 3 mendelian syndromes), with an overall incidence of malformations of 61%.
Type
|
Anomalies (8% of cases) |
|
Cardiovascular |
|
|
Extracardiac
abnormalities |
|
|
Chromosome
anomalies (8%) |
|
HEMODYNAMICS |
Pulmonary blood flow is supplied retrograde through the ductus arteriosus
with absence of RV hypertrophy or IUGR.
POSTNATAL |
- The
variable resistance created by the stenotic pulmonary artery, prevents the
venous flow of the right heart from moving freely towards the pulmonary
circulation, and the wide interventricular defect allows it into the left
ventricle and aorta, creating the right to left shunt.
- In
utero, this is not a problem for the fetus, since normal blood oxygenation
takes place in the utero-placental unit.
- In
the classic Fallot, systemic hypoxia is the most important problem after
birth and the admixture explains the cyanosis in the affected individuals.
- The
severity of both, the pulmonary artery stenosis and the aortic overriding
above the interventricular septum, will determine the degree of hypoxia
and cyanosis of the newborn.
- In
mild cases cyanosis may be absent.
- The
more severe the pulmonary stenosis the greater the size of the ascending
aorta (both aortic and pulmonary flow will be directed through it).
- After
birth, right ventricular hypertension and subsequent concentric
hypertrophy of the right ventricle occurs due to:
- the
right ventricle is subjected to the left ventricular and aortic pressures
due to the large interventricular septal defect
resistance to flow due to the pulmonary stenosis
PROGNOSIS |
In early life the prognosis will be determined by the
presence of associated anomalies and fetal syndromes in which cases the
survival rate is only 10%. In isolated cases of tetralogy of Fallot, the
survival rate reaches 85%.
Those cases with severe pulmonary
stenosis or atresia, aneurysm of the pulmonary artery associated with hydrops
fetalis and polyhydramnios, and great overriding aorta above the
interventricular septal defect, will eventually have cardiac failure and may
die in utero. Those that do not die in utero will be cyanotic after birth and
will have short life expectancy.
Those cases of mild to moderate
pulmonary stenosis with discrete overriding aorta will have the best prognosis
and surgical results. The cyanosis after birth may be gentle or absent, and a
normal life span may be achieved.
Recurrence risk: In cases of a sibling with Tetralogy
of Fallot, the recurrence risk is estimated in 2%.
REFERENCES |
- Kleinman CS, Donnerstein RL, DeVore GR et.al. Fetal echocardiography for evaluation of in utero congestive heart failure. N Engl J Med 1982;306:568-575.
- Sanders SP, Bierman FZ, Williams RG. Conotruncal malformations: diagnosis in infancy using subxiphoid 2-dimensional echocardiography. Am J Cardiol 1982;50:1361-1367.
- DeVore GR, Siassi B, Platt LD. Fetal echocardiography VIII. Aortic root dilatation - a marker for tetralogy of Fallot. Am J Obstet Gynecol 1988;159:129-136.