|
HEMANGIOMA HEMANGIOENDOTHELIOMA |
The terms arteriovenous malformation, infantile hemangioma (capillary or
cavernous), and hemangioendothelioma are used synonymously to describe vascular
hepatic tumors described before 6 months of age (1). It is the most common
symptomatic vascular tumor of infancy, with 85% presenting in the first 6
months of life. There is a female
predominance 967%). They are considered benign tumors of vascular origin, but
they do have a high frequency of malignant degeneration (sarcomas). Cutaneous
hemangiomas may be present in 45% of cases and the alpha fetoprotein may
occasionally be increased. The main complication is congestive heart failure
due to arteriovenous shunting.
|
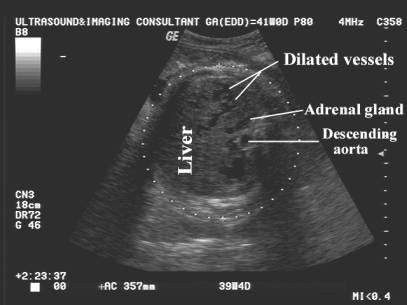
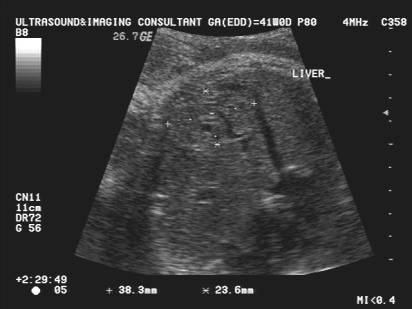
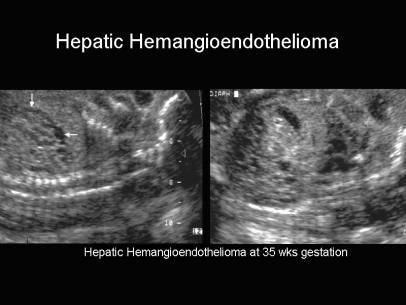
Ultrasound Prenatal detection of an arteriovenous malformation is important intrauterine steroid therapy and careful prenatal planning is required, as about 50% of infants have high output congestive cardiac failure as the presenting feature (2). |
|
|
Hypoechoic mass and usually well
circumscribed. Solitary lesions are more common than multiple lesions. It may less commonly be isoechoic or hyperechoic (this generally occurs as the tumor fibrosis and involutes). |
|
|
|
|
|
·
Congestive cardiac
failure (4). |
|
|
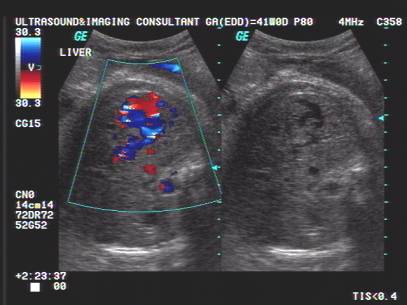
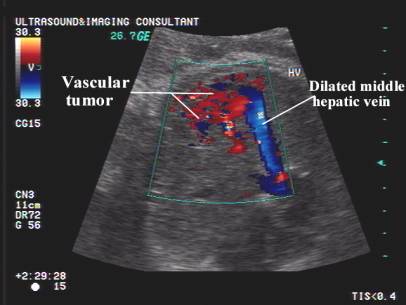
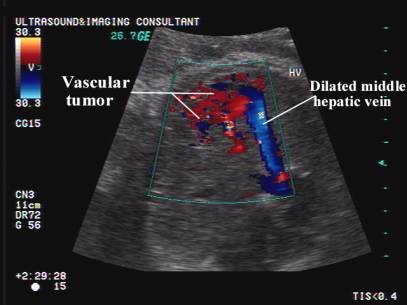
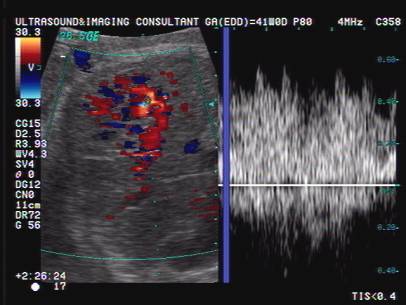
Color doppler usually demonstrates a large
vessel with bidirectional flow feeding into a complex hypoechoic mass. |
|
|
|
|
|
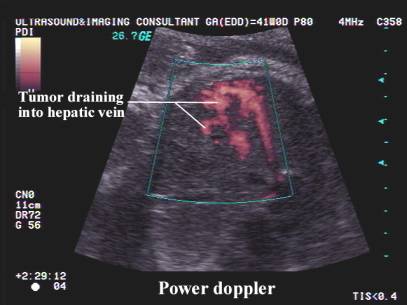
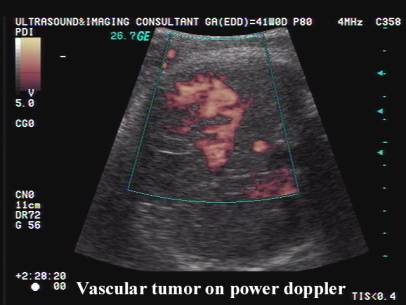
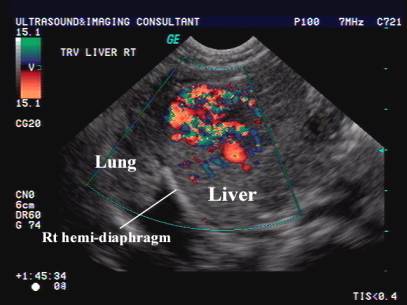
Power doppler demonstrates a vascular tumor
that drains into the middle hepatic vein. |
|
|
|
|
|
Arteriovenous lakes demonstrate high velocity
flow patterns with a mixed arterial and venous pattern. High velocity
waveforms have been reported in the hepatic veins (5). |
|
|
|
|
|
Post-natal abdominal ultrasound: Vascular mass in liver. |
|
|
|
|
|
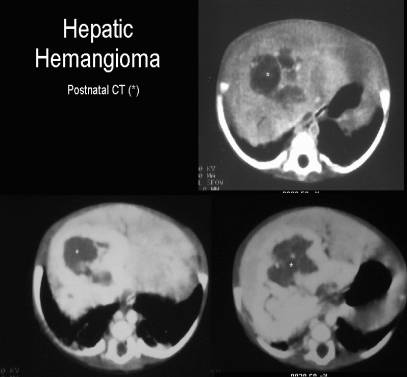
Post-natal CT scan through the liver: Mass seen on non-contrast enhanced scan
(upper panel). Marked vascular enhancement on the post
contrast scans (lower panels). |
|
|
|
|
|
Differential diagnosis: 1. Mesenchymal hamartoma. 2. Cavernous hemangioma. 3. Hepatoocelluar carcinoma. 4. Hepatoblastoma. 5. Metastatic neuroblastoma. |
|
REFERENCES |
- Paltiel HJ, Patriquin HB, Keller MS et.al. Infantile hepatic hemangioma: Doppler ultrasound. Radiology 1992;182:735-742.
- Stanley P, Geer GD, Miller JH et.al. Infantile hepatic hemangiomas: clinical features, radiologic investigations, and treatment of 20 patients. Cancer 1985;64:936.
- Petrovic O, Haller H, Rukavina B et.al. Prenatal diagnosis of a large liver cavernous hemangioma associated with polyhydramnios. Prenat Diagn 1992;12:70.
- Gonen R, Fong K, Chiasson DA. Prenatal sonographic diagnosis of hepatic hemangioendothelioma with secondary non-immune hydrops. Obstet Gynecol 1989;73:485-487.
- Abuhamad AZ, Lewis D, Inati M et.al. The use of color doppler in the diagnosis of fetal hepatic hemangioma. J Ultrasound Med 1993;4:223-226.
- Berger TM, Berger MF, Hoffman AD et.al. Imaging diagnosis and follow-up of infantile hemangioendothelioma: a case report. Eur J Pediatr 1994;156:100-102.
- Selby DM, Stocker JT, Waclawiw WA et.al. Infantile hemangioendothelioma of the liver. Hepatology 1994;20:39-45.