|
PYELECTASIS |
Mild pyelectasis is diagnosed when:
· The renal pelvis anteroposterior diameter is greater than 4 or 5 mm and less than 10 mm.
· Corteville et al (1) in a study evaluating the ability of six different ultrasonographic parameters to predict postnatally confirmed congenital hydronephrosis, found that an:
1. anteroposterior diameter of greater than or equal to 4 mm before 33 weeks and greater than or equal to 7 mm after 33 weeks had a sensitivity of 100%, but a false-positive rate of 21% to 55% (depending on the gestational age).
2.
If one is screening for Down syndrome, however, it is
preferable to minimize the false-positive rate to less than 5% so as to avoid
unintended fetal loss as a result of invasive procedures. Corteville
et al (2), using the parameters of greater than or equal to 4 mm before 33
weeks and greater than or equal to 7 mm after 33 weeks, found the overall
sensitivity of pyelectasis for the detection of Down syndrome to be 17%. This
dropped to 4% when pyelectasis was an isolated finding. The false-positive rate
in this series was 2%, with a positive predictive value of isolated pyelectasis
for
1. DEFINITION OF PYELECTASIS VARIES FROM AUTHOR TO AUTHOR |
|
Gestational age-based criteria for the diagnosis of fetal renal pyelectasisa |
||
ULTRASOUND
|
· 3 to 11 mm in 18% of routine examinations (17).
· Theories as to causes include maternal hormone influence and maternal volume expansion (14).
- Of 20 fetuses, 70% had both normal (which they defined as an AP measurement of <4 mm) and abnormal values.
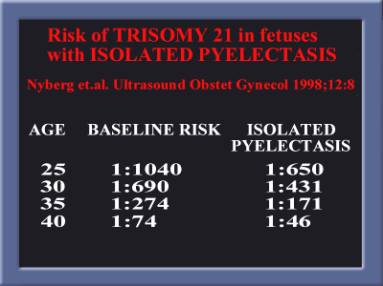
- There is an increased incidence of mild pyelectasis (>4 mm) among fetuses with Down’s syndrome (27).
- A recommendation, however, for amniocentesis requires other associated abnormal anatomical findings or risk factors (eg, advanced maternal age) before risking possible fetal demise from the amniocentesis itself (2).
· Fetal pyelectasis is more often bilateral,
· When unilateral it is more likely to be on the left side (11,12).
· It is more common in male fetuses both prenatally and postnatally (1,11, 7,4,13).
· Laterality does not seem to be useful for prognosis.
2. ISOLATED FETAL PYELECTASIS |
|
Regression
lowers the risk but does not completely eliminate it. |
Down
syndrome |
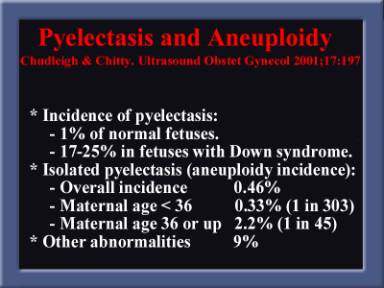
PYELECTASIS
AND ANEUPLOIDY
|
PYELECTASIS
AND POSTNATAL RENAL ABNORMALITIES
|
· Sixty-two percent of fetuses (42% of all kidneys) had postnatal renal abnormalities.
LONG
TERM OUTCOME
|
|
Outcome
by age 4 of fetuses with prenatally diagnosed bilateral pyelectasis |
||||
Mild |
||||
Moderate |
||||
Severe |
||||
3. CORRELATION BETWEEN PELVIS SIZE AND BLADDER VOLUME |
4. SONOGRAHIC APPROACH TO PYELECTASIS |
REFERENCES |
- Corteville
JE, Gray DL, Crane JP. Congenital hydronephrosis: correlation of fetal
ultrasound findings with infant outcome. Am J Obstet Gynecol
1991;165:384-8.
- Corteville
JE, Dicke JM, Crane JP. Fetal pyelectasis and Down syndrome: is genetic
amniocentesis warranted? Obstet Gynecol 1992;79:770-2.
- Benacerraf
BR, Mandell J, Estroff JA, Harlow BL, Frigoletto F. Fetal pyelectasis: a
possible association with Down syndrome. Obstet Gynecol 1990;76:58-60.
- Adra
AM, Mejides AA, Dennaoui MS, Beydoun SN. Fetal pyelectasis: is it always
“physiologic”? Am J Obstet Gynecol 1995;173:1263-6
- Langer
1996
- Wickstrom
E, Maizels M, Sabbagha RE, Tamura RK, Cohen LC, Pergament E. Isolated
fetal pyelectasis: assessment of risk for postnatal uropathy and Down
syndrome. Ultrasound Obstet Gynecol 1996;8:236-40.
- Chudleigh
T. Mild pyelectasis. Prenat Diagn 2001;21:936-41
- Broadley
P, McHugo J, Morgan I, Whittle MJ, Kilby MD. The 4 year outcome following
the demonstration of bilateral renal pelvic dilatation on pre-natal renal
ultrasound. Br J Radiol 1999;72:265-70.
- Ismaili
K, Hall M, Donner C, Thomas D, Vermeylen D, Avni FE. Results of systematic
screening for minor degrees of fetal renal pelvis dilatation in an
unselected population. Am J Obstet Gynecol 2003;188:242-6.
- Bobrowski
RA, Levin RB, Lauria MR, Treadwell MC, Gonik B, Bottom SF. In utero
progression of isolated renal pelvis dilation. Am J Perinatol
1997;14:423-6.
- Havutcu
AE, Nikolopoulos G, Adinkra P, Lamont RF. The association between fetal
pyelectasis on second trimester ultrasound scan and aneuploidy among 25
586 low risk unselected women. Prenat Diagn 2002;22:1201-6
- Chudleigh
PM, Chitty LS, Pembrey M, Campbell S. The association of aneuploidy and
mild fetal pyelectasis in an unselected population: the results of a
multicenter population. Ultrasound Obstet Gynecol 2001;17:197-202.
- Persutte
WH, Koyle M, Lenke RR, Lkas J, Ryan C, Hobbins JC. Mild pyelectasis
ascertained with prenatal ultrasonography is pediatrically significant.
Ultrasound Obstet Gynecol 1997;10:12-8.
- Petrikovsky
BM, Cuomo MI, Schnieder IP, Wyse LJ, Cohen HL, Lesser M. Isolated fetal
hydronephrosis: beware the effect of bladder filling. Prenat Diagn
1995;15:827-9.
- Graif
M, Kessler A, Hart S, Daitzchman M, Mashiach S, Boichis H, et al. Renal
pyelectasis in pregnancy: correlative evaluation of fetal and maternal
collecting systems. Am J Obstet Gynecol 1992;167:1304-6.
- Allen
KS, Arger PH, Mennuti M, Coleman BG, Mintz MC, Fishman M. Effects of
maternal hydration on fetal renal pyelectasis. Radiology 1987;163:807-9.
- Hoddick
WK, Filly RA, Mahony BS, Callen PW. Minimal fetal renal pyelectasis. J
Ultrasound Med 1985;4:85-9.
- Robinson
JN, Tice K, Kolm P, Abuhamad AZ. Effect of maternal hydration of fetal
renal pyelectasis. Obstet Gynecol 1998;92:137-41.
- Nicolaides
KH, Cheng HH, Abbas A, Snijders RJM, Gosden C. Fetal renal defects:
associated malformations and chromosomal defects. Fetal Diagn Ther
1992;7:1-11.
- Wickstrom
EA, Thangavelu M, Parilla BV, Tamura RK, Sabbagha RE. A prospective study
of the association between isolated fetal pyelectasis and chromosomal
abnormality. Obstet Gynecol 1996;88:379-82.
- Guariglia
L, Rosati P. Isolated mild fetal pyelectasis detected by transvaginal
sonography in advanced maternal age. Obstet Gynecol 1998;92:833-6.
- Snijders
RJM, Sebire NJ, Faria M, Patel F, Nicolaides KH. Fetal mild hydronephrosis
and chromosomal defects: relation to maternal age and gestation. Fetal
Diagn Ther 1995;10:349-55.
- Bromley
B, Lieberman E, Shipp TD, Benacerraf BR. The genetic sonogram: a method of
risk assessment for Down syndrome in the second trimester. J Ultrasound
Med 2002;21:1087-96.
- Grignon
A, Filion R, Filiatrault D, Robitaille P, Homsy Y, Boutin H, et al.
Urinary tract dilatation in utero: classification and clinical
applications. Radiology 1986;160:645-7.
- Broadley P, McHugo J, Morgan I, Whittle MJ, Kilby MD. The 4 year outcome following the demonstration of bilateral renal pelvic dilatation on pre-natal renal ultrasound. Br J Radiol 1999;72:265-7
- W.H. Persutte, M. Hussey, J. Chyu et al., Striking findings concerning the variability in the measurement of the fetal renal collecting system. Ultrasound Obstet Gynecol 15 (2000), pp. 186–190.
- B.R. Benacerraf, J. Mandell, J. Estroff et al., Fetal pyelectasis: A possible association with Down syndrome. Obstet Gynecol 76 (1990), pp. 58–60.