|
CLASSIFICATION OF
FETAL HYDRONEPHROSIS (1) |
|
Pyelectasis |
Calectasis |
Pyelectasis |
|
|
|
|
|
Grade |
Calyceal Dilatation |
Size of Renal Pelvis (Antero-posterior
diameter) |
|
I |
Physiological
dilatation |
1 cm |
|
|
Grade
1 |
|
|
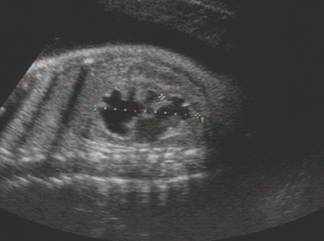
Pyelectasis 8 mm No caliectasis |
|
|
|
|
Grade
2 |
|
|
|
|
|
|
|
Grade
3 |
|
|
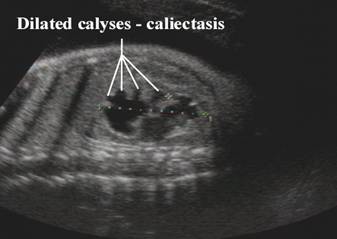
Pyelectasis Caliectasis No cortical atrophy |
|
|
|
|
Grade
4 |
|
|
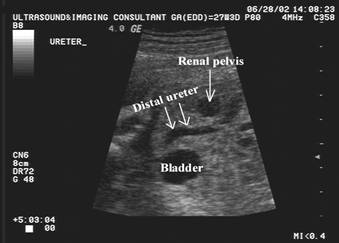
Pyelectasis Caliectasis Ureteric dilatation |
|
|
|
|
Grade
5 |
|
|
|
|
|
|
|
|
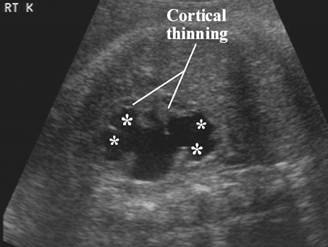
Pyelectasis Severe caliectasis Cortical atrophy Ureteric dilatation |
|
|
|
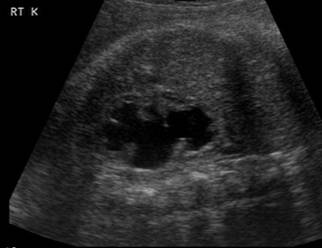
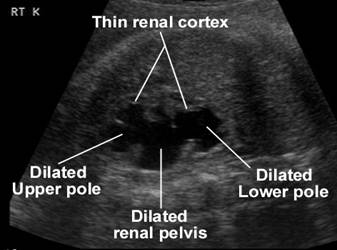
Hydronephrosis 28 weeks Dilated renal pelvis Global cortical loss |
|
|
|
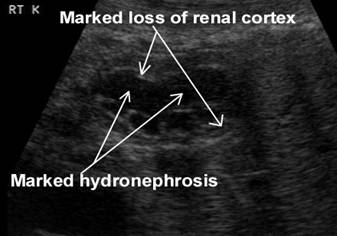
Same case at 34 weeks Hydronephrosis Severe global cortical loss |
- Grignon et al (1) developed a grading system for hydronephrosis in fetuses of 20 weeks gestation or greater in relation to their postnatal findings. Grade I dilatations (AP renal pelvic diameter up to 1.0 cm) were described as normal and physiologic because none of the affected patients required surgery after birth. Grade II (>1.0–1.5 cm) and grade III (>1.5 cm with slight dilatation of calices) dilatation was termed intermediate hydronephrosis; 50% required postnatal surgical intervention. All patients with grade IV dilatation (>1.5-cm pelvis, moderate dilatation of calices, no cortical atrophy) or grade V hydronephrosis (>1.5-cm pelvis, severe caliceal dilatation, atrophic renal cortex) required surgery. Their work suggests that one should be concerned with pelvic dilatations greater than 10 mm particularly if there is associated calyceal dilatation and loss of cortex.
- Corteville et al (2) pointed out that one should be concerned with lesser degrees of dilatation in fetuses younger than 23 weeks gestation because these dilatations may be proportional to larger dilatations in the larger kidneys of older fetuses.
- Langer et al (3) found 89 (4.4%) of 2170 fetuses with significant renal pelvic dilatation (described as >5 mm if 28 weeks or less and >10 mm if >28 weeks). Only 13.7% had postnatal obstruction, reflux, or primary megaureter as the cause. 30.5% had pyelectasis without obstruction and 55.8% had no abnormality after delivery. They concluded that one should not consider a pelvis abnormally dilated if <10 mm after 28 weeks gestation, unless there is concurrent bladder or ureteral dilatation.
- Dremsek et al (4) found prenatal determinations for dilatation less helpful than postnatal measurements and suggested no need for concern in a neonate with a renal pelvis AP measurement of <10 mm.
- Degani et al (5) found 67% of 420 mothers who bore a child with 4 mm or > antenatal renal pelvic dilatation also had a fetus with pelvic dilatation in their next pregnancy. They suggested a genetic or environmental influence as the cause of the 6.1 times greater than normal "risk" for mild pelvic dilatation among siblings.
In the neonatal assessment of antenatal pyelectasis versus hydronephrosis, one must be aware that there is a relative hypovolemia in the first day of life. A false-negative
result may occur when "emergency"
DIFFERENTIAL DIAGNOSIS |
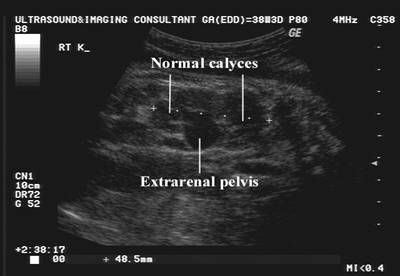
A prominent extra-renal pelvis may give the appearance that there is renal pyelectasis.
|
|
|
REFERENCES |
- Grignon A, Filion A, Filiatrault D et.al. Urinary tract dilatation in utero: classification and clinical applications. Radiology 1986;160:645-647.
- J.E. Corteville, D.L. Gray and J.P. Crane, Congenital hydronephrosis: correlation of fetal ultrasonographic findings with infant outcome. Am J Obstet Gynecol 165 (1991), pp. 384–388.
- B. Langer, U. Simeoni, Y. Montoya et al., Antenatal diagnosis of upper urinary tract dilation by ultrasonography. Fetal Diagn Ther 11 (1996), pp. 191–198.
- P. Dremsek, K. Gindl, P. Voitl et al., Renal pyelectasis in fetuses and neonates—Diagnostic value of renal pelvic diameter in pre- and postnatal sonographic screening. Am J Roentgenol 168 (1997), pp. 1017–1019.
- S. Degani, Z. Leibovitz, I. Shapiro et al., Fetal pyelectasis in consecutive pregnancies: A possible genetic predisposition. Ultrasound Obstet Gynecol 10 (1997), pp. 19–21.
- H.L. Cohen and J.O. Haller, Diagnostic sonography of the fetal genitourinary tract. Urol Radiol 9 (1987), pp. 88–98.